By Maria Biasutti
I had the privilege recently to meet two residents living in a long term care home who were passionate about food, but unfortunately had shared with me lists of what we always coin the term as “complaints”. One resident used to be an SLP who worked with children for 40 years, while the other resident used to work as an executive chef in senior living. As dietitians in LTC, where we spend most of our days documenting, we’re not often graced with the time to speak to residents enough to get to know who they really are. I was very lucky to spend a combined 2 hours with both of them. Unfortunately, they came to me angry, frustrated and feeling unheard.
The situation, from their perspective, was an “us versus them”. They even told me that they were fortunate to still be able to speak and express themselves and what they like to eat, while they can see many others who could not – to which they felt the responsibility to speak for. The resident who was an SLP emphasized many times during our conversation, “ever heard the F-word? It means FRESH! Something we don’t get enough of here!”. For this resident and the children they used to treat for SLP therapy, the “F-word” used to stand for “FUN”. I learned that this resident’s family used to run a produce market and sell their produce to Wendy’s in the earlier days when Wendy’s first came to Canada. The resident and their family would wake up early in the morning to drive to the Toronto Food Terminal to select the juiciest tomatoes and the greenest, crispiest lettuce several times a week… so that Wendy’s customers can enjoy a fresh salad with their hamburgers. This is why the “F-word” was reiterated several times and now there’s no way I’ll forget it.
On my drive home, this resident was all I thought about. I realized the resident’s request for a personal salad every day was because if there was nothing else they wanted to eat from the menu choices of the day, they were already prepared not to go hungry. But the way staff saw it instead, was that the salad was just another thing they had to add to their already busy prep schedule.
Reflecting deeper, I wondered how things could be changed to support this resident so that their personal food label for a salad will never be taken away? That it would never be replaced by something else that they may not want. It may be easier for us as dietitians to recognize that someone is losing weight and we make the quick decision to give them a supplement. Perhaps, the real solutions should come from asking questions like:
“Well, does the food actually taste good?”
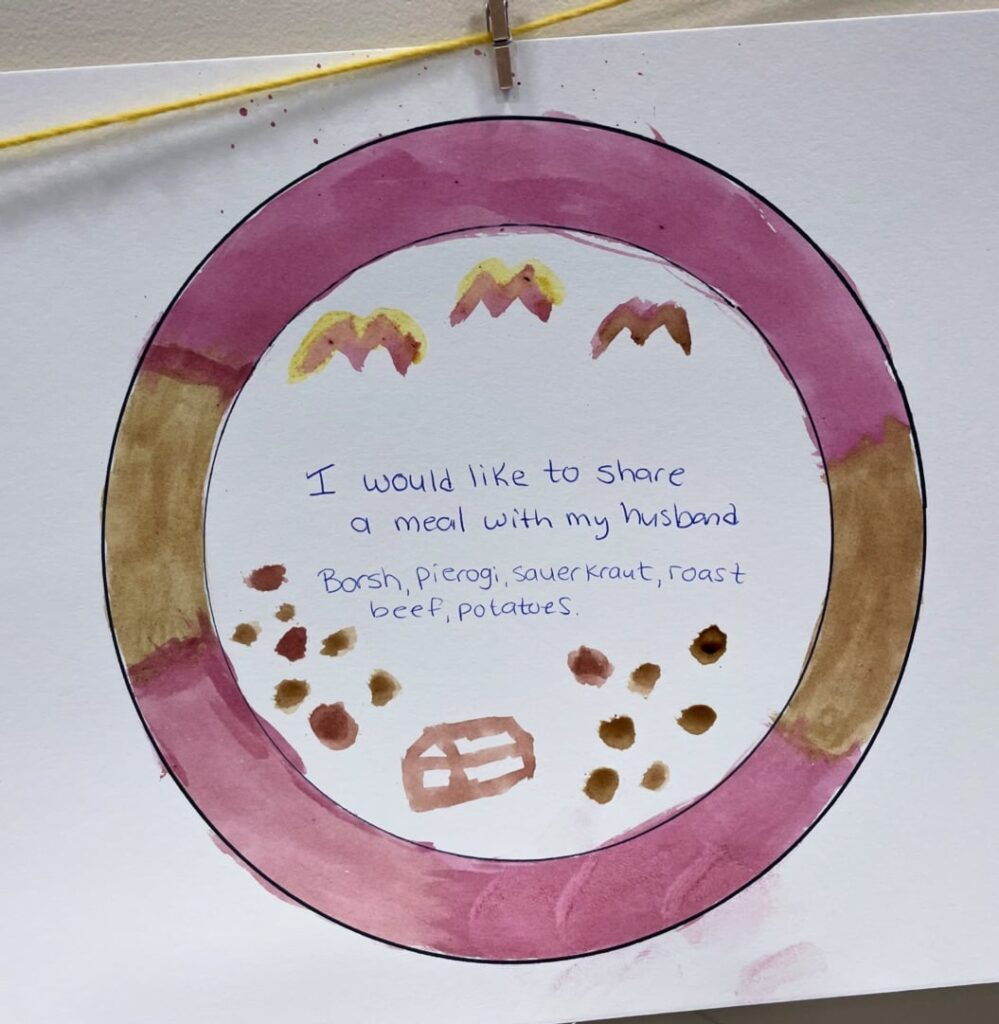
“What did this resident enjoy eating before coming to LTC? And is there any way to get it?”
“What does food mean to you?”
“How would you like to eat this meal?”
In our own professional toolboxes, we can sharpen and strengthen our tools by understanding what it truly means to respect a resident’s choice. We can do this by asking challenging questions to ourselves and others (ie. well, why and why not?) or sometimes having those difficult and emotional conversations (ie. end of life). Yes, we should remember the science and the evidence, but near the end of life, it’s always about humanizing the experience.
If you like my story, but need more best practices, here’s some info for you: Reference
